|
|
|
|
|
| |
Quality general dental care with an emphasis on natural esthetics, form and function. Experience with complex restorative, prosthetic and implant treatment.
----------------------------------------------------------------------------------------
ENDODONTICS (ROOT CANALS): SAVING TEETH
What is a root canal?
A tooth is composed of a crown (the part that is visible to your eye) that is attached to the root (portion that is within the bone and not visible). The crown of the tooth is covered by enamel a hard crystalline substance. The enamel is very hard and allows us to chew food without wearing the tooth away. Under the enamel and composing the root is dentin. Dentin, is a softer organic substance that is composed of tubules that run between the pulp and enamel and contain a nerve fiber. The pulp is housed within the dentin and is composed of nerves and blood vessels (called the pulp).
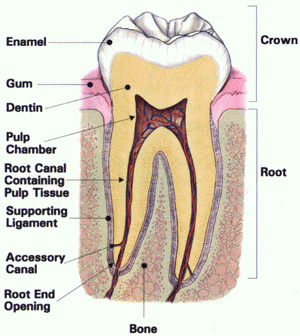
The pulp comprises the "root canal" system of the tooth. When decay progresses through the enamel into the dentin, bacteria are carried into the dentinal tubules. The bacteria can cause an infection in the pulp causing the pulpal tissue to become inflammed and painful.
Why do I feel pain?
The only nerve fibers in the pulp are pain fibers. So, any sensation within the pulp is felt as pain. Since the pulp is housed within a hard shell (the dentin), when any inflammation occurs the pulpal tissue swells and strangulates the vessels causing the pulp to die. bacteria that are within the pulp tissue are now able to multiply as the body is unable to bring white blood cells into the tissue to fight the infection. When the pulp tissue is vital, meaning there is some life in it, pain will be felt as the inflammation begins which is a warning that a problem has occurred. But when a tooth is nonvital (the pulpal tissue has been dead for a period of time) or the infection has progressed, pain will be felt when the infection spreads out the apex (tip) of the root. This is referred to as an abscess. When an abscess progresses and begins to drain into the mouth it is referred to as a fistula.
Why do I need root canal therapy?
An infection within the pulp can not heal itself and if left untreated can cause the tooth to be lost or if the infection spreads may lead to a life threatening situation. When a tooth becomes infected the options are to extract the tooth or save the tooth with root canal therapy. Though an extraction is cheaper, the space left behind will require an implant or a bridge, which can be more expensive than root canal therapy. It is better to maintain your own teeth verses replacing them through bridges, implants or dentures. Root canaled teeth can last for many years following treatment.
What is involved in root canal therapy?
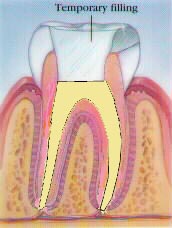
Once it has been determined that the tooth has an infection and requires root canal therapy, it is necessary to determine if the tooth once treated by a root canal can be restored and returned to function. If the tooth can be restored, the tooth is given a local anesthetic to numb the area and make the treatment comfortable. The tooth is isolated. The decay is removed from the tooth and an access is made to permit entry into the pulp canals. The pulpal tissue and necrotic debris is removed and the canals cleaned. Depending on the condition of the tooth, the crown may be sealed temporarily to guard against recontamination, the tooth may be left open to drain, or the dentist may fill (obturate) the canals. If a temporary filling has been placed between appointments, on the next visit it is removed and the pulp chamber and canal(s) are filled with rubber like gutta percha or another material to seal the entire canal system and prevent recontamination.
What happens after the root canal is finished?
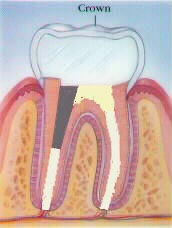
Once the root canal has been completed, the tooth needs to be restored. Depending on how much of the tooth remains will determine how it will be restored. Generally, if there is only a small area of decay and a majority of the tooth remains (seen usually with anterior teeth) the access opening and missing tooth can be restored with a bonded filling. When less than 50% of the crown is missing an onlay may be used to restore the tooth to full function. But, if there is more than 50% of the tooth to be replaced a post & core needs to be placed and full coverage crown placed to prevent the tooth from being fractured during chewing.
What are the risks and complications?
More than 95 percent of root canal treatments are successful. However, sometimes additional treatment is needed to remove the infection. The root canal system is composed of large canals that are visible on x-rays and very fine canals that can not be seen on x-rays. Sometimes the fine canals at the tip of the root are unable to be cleaned during the root canal procedure and surgery is needed to seal the tip of the root (apex) from outside the tooth. Other times a fine canal may flare up and necessitate redoing the root canal to achieve a better seal. It is also possible that the root may have a fracture or develop a fracture if not restored necessitating removal of the tooth.
What if the root canal becomes reinfected or continues to cause me pain?
In about 5% of teeth that have undergone root canal therapy further treatment may be necessary to seal the tooth and remove the infection at the roots tip. The tip of the root not only has the main canal that is visible on an x-ray but has many fine canals forming an anastomosis. These fine canals are too small and numerous to be instrumented. When the infection that lead to the need for a root canal persists or reoccurs, Endodontic surgery may be needed to seal the anastomosis. This consists of exposure of the root tip, "clipping" the root tip to remove the anastomosis, sealing the root tip with a "retro grade filling" and curetting any cystic tissue from the area.
What happens after treatment?
Natural tissue inflammation may cause discomfort for a few days, which can be controlled by an over-the-counter analgesic. A follow-up exam can monitor tissue healing. From this point on, brush and floss regularly, avoid chewing hard foods on the treated tooth, and see your dentist regularly.
Stages of Root Canal Therapy:
Step 1: Decay is removed to expose the pulpal tissue and allow access into the canals.
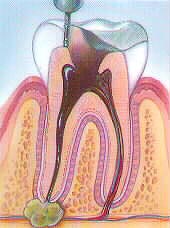
Step 2: The pulpal tissue is removed with special files.
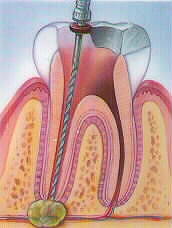
Step 3: The canals are shaped to allow obturation of the root canal system. This may be completed in a single visit or require several visits depending on the health of the tooth and the access to the apex of the root.
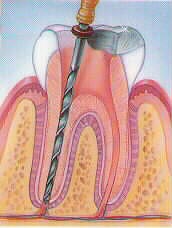
Step 4: The canals are obturated (yellow), completing the root canal and is ready to be restored.
Step 5: The missing tooth structure is replaced and the tooth is returned to function.
Implant Cosmetic Dental Center™
----------------------------------------------------------------------------------------
Dr. Gregori M. Kurtzman is an international lecturer, selected as one of the top 100 dental speakers since 2006 by Dentistry Today, author of over 200 professional articles, a consultant to multiple dental manufacturers for product evaluation, development and research, he provides general dental care in suburban Maryland since 1986.
|
|
|
|
|
|
|
|
|